Hip arthroplasty in obese patients: rising prevalence–standard procedures?
Michael Skutek, Nils Wirries, Gabriela von Lewinski • Annastift Hospital, Medical School Hannover, Germany
Abstract
We examined our experience and, in partic-ular, complications associated with total hip arthroplasty in obese and morbidly obese patients. We prospectively gathered 50 patients in a matched control series including 25 obese and morbidly obese patients. All patients were operated using the direct lateral approach and standard postoperative protocols. Operating room time, complications, disloca-tions, blood loss, cup position and clinical parameters using the Harris Hip Score and the Western Ontario and McMaster Universities Arthritis Index results were compared. Although there were some significant differ-ences in clinical outcomes, standard proce-dures yielded good overall results and an acceptable rate of complications. Details approaching this patient entity are being dis-cussed.
Introduction
The prevalence of obesity has risen substan-tially in Germany over the last 10 years. Using the calculated body mass Index (BMI), obesity is defined as a BMI ≥30 kg/m2. According to the German Health Interview and Examination Survey for Adults (DEGS1), conducted from 2008 through 2011, the prevalence of over-weight (BMI ≥25 kg/m2 remained with 67.1%of men and 53.0% of women the same over the last years. However current data present a sub-stantial increase of obese men from 18.9% to 23.3% and in women from 22.5% to 23.9% com-pared to the previous survey in 1998.1 The increase in obesity occurred especially among young adults.1,2 Simultaneously higher BMI lead to endoprosthetic treatment in younger age, which is carried out at significantly lower levels of preoperative joint function.3
Previous studies and current meta analyses report a higher risk of total hip replacements (THA) when being performed in obese patients. Factors associated with THA in these patients and potential complications comprise increased risk for re-operation and infection,4-6 prolonged operating room (OR) time,7,8 expectations of poorer clinical outcomes,9 risk of component malpositioning10 and risk of dislocation.11 In order to reduce these risks, measures such as pre-operative weight loss regimes12 and avoid-ing the use of minimally invasive approaches have been advocated.13,14
Given the current prevalence of obesity in Germany, we undertook a closer observation of our current standard procedure for THA. We queried, if obesity with an BMI >30 kg/m2 affected the results of THA in our patients compared to patients without obesity (BMI <30 kg/m2) and whether there was a need to alter procedures or decision making in this group?
Materials and Methods
Fifty consecutive patients with severe osteoarthritis were identified performing a match-control analysis (09/2011-09/2013). There were 18 men and 32 women. The mean age was 65±11 years at the time of operation. All patients suffered from primary osteoarthri-tis either with normal or dysplastic hip joints. Patients were referred to a referral center for total joint replacement (TJR) and operated by a single surgeon or a resident under direct supervision. Twenty-five consecutive patients with a BMI >30 kg/m2 were included and matched to the next consecutive patient with a BMI <30 kg/m2. Patients were graded using the WHO scheme into normal and overweight grade 1-3, also called simple overweight – BMI of 25-29.9 kg/m2, obesity –BMI of 30-39.9 kg/m2 and morbid obesity – BMI 40 kg/m2. IRB was consulted (No. 2989-2015).
The operative technique and implants were the same both in overweight and (morbidly) obese patients. The direct lateral approach as described by Hardinge was used. Patients were prepped and draped in the lateral decubitus position using an additional iodine draping. Cefuroxime single shot prophylaxis was administered with adapted dosage in morbidly obese patients. Jet lavage was used in all cases. The Implant was a press fit cementless implant using a delta ceramic head (32 mm) and a cross-linked polyethylene insert. Fluoroscopy was applied in all cases, after plac-ing the definitive cup and before inserting the definitive stem with a trial rasp instead. This was done to leave options for small corrections of the press fit cup and to adjust the size and position of the stem and also to optimize the offset and leg length. We used wound dressing consisting of a highly absorbent pad, maximiz-ing the passage of blood and exudate into the dressing, minimizing the risk of fluid strikethrough. Therefore reducing the need for dressing changes.
OR time, fluoroscopy time, pre and postoper ative hemoglobin levels, postoperative cup inclination (aimed between 30-45° inclina-tion) was noted. At final follow up, the Harris Hip Score (HHS) and a modified Western Ontario and McMaster Universities Arthritis Index (WOMAC) (max. 100 pt. = excellent) were calculated. Statistics comparisons were made using the t-test (two tailed) and P<0.05. Potential complications (wound dehiscence, infection, dislocation, DVT) were noted.
Results
According to the WHO grading, there were 20 obese patients and 5 morbidly obese patients, adding up to 25 patients with a mean BMI of 38±4 kg/m2 (group A). In the matched control group, there were 9 patients with nor-mal weight and 16 overweight patients adding up to 25 patients in control group B. The mean BMI of 27±2 kg/m2 (Table 1). After a mean fol-low-up of 30±6 months, overall satisfaction was similar in Group A and B. On a scale from 1 (very satisfied to 10 not satisfied) there was a mean of 1.6±0.6 in group A and 1.8±0.6 in group B. Patients who were working were able to return to their respective work after 3 months regardless of BMI. There was no post-operative Trendelenburg gait in either group. Postoperatively, there were no deep vein thromboses, dislocations or general medical complications. Hemoglobin dropped from a preoperative level of 13.9±0.6 g/dL to a postop-erative level of 10.6±0.8 g/dL in Group A and from 13.8±1 g/dL to 10.2±0.6 in Group B, demonstrating no significant difference (P>0.05). No patient in either group required blood transfusion.
Overall post-operative outcome score results improved in both groups. In group A from pre-op 38±6 to post-op 89.5±7 (WOMAC) and 36.8±6.2 to 87.9 (HSS). Both increases were statistically significant (P<0.01, Table 2). Similar increase was noted in Group B from pre-op 49.6±11 to 93±8 (WOMAC) and 48.8±12 to 92±6 (HHS). Again the increase was statistically significant (P<0.01, Table 2).
The HHS showed significantly better results in the non-obese group B (92±6 vs. 87±9, P=0.02, Table 2). The WOMAC also improved more in non-obese group B patients though not reaching statistical significance (89.5±7 vs. 93±8, P=0.2). Interestingly the pre-op WOMAC and HHS scores were significantly decreased in the obese group A, compared to the non-obese group B (P=0.01, WOMAC and HHS).
In the obese Group A there was also a signif-icant longer skin incision in total 23±4 cm vs. 14±1.3 cm, P<0.05 (Figure 1, Table 3). Also OR time was significantly increased in group A (92±18) vs. group B (77±10, P<0.01). Similar tendencies were observed by Bennet.15 Some authors noted an increased utilization of operating room time in patients with increased BMI during primary total hip arthro-plasty.7,8,15 That in turn might contribute to an increased risk of infection as noted by Belmont. He found that morbid obesity (P<0.001) and operative time >141 minutes (P<0.001) were strongly associated with the development of major local complications.5 Compared to these data, the OR time for obese and morbidly obese patients was relatively low (92±18 minutes, Table 3). Even in morbid obese Patients OR times less than 80 minutes were possible.
One obese Patient (m, BMI 34) developed a superficial skin infection following wound dehiscence while training on an ergometer 2 weeks post surgery. Prophylactic antibiotics were given. The skin healed uneventfully, with no need for revision surgery.
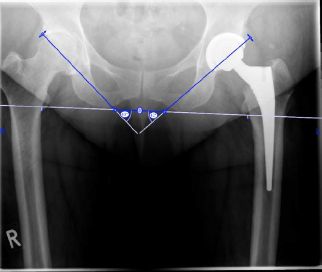
Given our results, OR time was moderately longer in obese and MO patients. In this series we had no infections though our numbers were small. The incidence should change with increased numbers necessarily. No significant differences were noted in terms of cup inclina-tion (Table 3, Figure 2). The standard expo-sure ensures correct sizing and placement of the cup under direct vision and also allows access for correct insertion of the appropriate-ly sized stem without compromising soft tis-sue, bone or tendons. This has happened in some minimally invasive techniques, though.16 There is no role for minimally invasive tech-niques in this patient cohort, and we support this approach. Another patient had a meralgia paresthetica in the contralateral hip (f, BMI 37), which dissolved after 7 months. This has been described in other studies and is thought to be related to the lateral decubitus position.17 In neither group were there DVT, dislocations or general medical complications at latest follow-up.
Discussion and Conclusions
The aim of this study was to assess the dif-ference between obese and non-obese patients with respect to intra-operative and post-opera-tive complications and post operative outcome scores for total hip arthroplasty. This is cur-rently of particular relevance as the degree of obesity in the German community continues to increase, and predictions for our future requirement for total hip arthroplasty are to increase.18,19
Using our standard direct lateral approach for THA in obese patients we observed differ-ences in the OR time, which was increased in obese and morbidly obese patients, however still with mean operative time close to 90 min-utes. We also noted a longer skin incision, which we do not hesitate to use as necessary to make the access, view and operative time as favorable as possible. We definitely counsel against minimal invasive approaches.
The increased risk of infection should not be a barrier in these patients. Although there is ample evidence for increased infection and related problems in obese and MO patients,4,6 other data show that THA can be safely per-formed in these patients with minimal increased risk, and this is supported by our data.
Using the direct lateral approach, a con-trolled extension of the skin incision when necessary provides excellent access. We feel that standardized procedures, avoiding mini-mally invasive or other less extensile approaches, help to keep OR time low and to reduce related risks such as infection, compo-nent malposition or fracture. Informed consent should strongly emphasize the increased risk of infection preoperatively.
Of all variables considered, high BMI is the most significant risk factor leading to malposi-tioning and or instability.10,11,20,21 It is well rec-ognized that component malposition is a cru-cial contributor to early dislocation and long term complications such as aseptic loosen-ing.13 We feel that the use of intraoperative flu-oroscopy is a very useful adjunct to ensure cor-rect uncemented stem size fill, and appropriate cup orientation, and in our study, no outliers in inclination and or rotational malposition occurred. Using the DLA without excision of anterior capsule with subsequent closure con-tributes to initial hip stability16 and has low rates of instability. We had no abductor muscle repair failures, no Trendelenburg gaits and no dislocations in our study.
Nerve dysfunction has been reported in 2.8% using the DAA and is rarely seen in DLA. However having one patient with meralgia paresthetica on the contralateral site brings the focus to correct positioning and padding when operating in the lateral decubitus posi-tion.
After adjusting for covariates, the risk of SSI and readmission was not significantly differ-ent in the patients who gained or lost weight pre-operatively compared to those who remained the same in 4066 THAs (1/1/2008-12/31/2010).12
Even after surgery there appears to be a ten-dency to gain, rather than to loose weight. At 12month follow-up, 18 obese or morbidly obese patients (9%) had lost ≥5% of their pre-operative weight and 118 patients (25%) had gained ≥5% of their preoperative weight.22 Considering these we recommend professional help for pre-operative weight reduction, how-ever if these interventions fail, we then pro-ceed with THA. Patients with BMI >28 kg/m2 showed greater improvements in function and in the physical component of general health after THA.23 Although the clinical outcomes of pri-mary THA were poorer in the super-obese patients, it is encouraging that even in these patients, THA can have acceptable outcomes. However, these patients may benefit from a discussion with their orthopedic surgeons to develop realistic expectations from the out-comes of their arthroplasty procedure.9 While this is not a comparative study comparing other techniques with the standard proce-dures, we do plan to follow this cohort to assess medium and long term outcomes.
Our findings support those already pub-lished in the literature, that obese and morbid-ly obese patients benefit significantly from THA. It is our routine practice to inform obese patients about the known increased risks asso-ciated with THA surgery, and advocate weight loss therapy pre-operatively. This may include bariatric surgery such as sleeve gastrectomy. Never the less if surgery is performed in this patient group, acceptable outcomes can be achieved with low complication rates and improved quality for patients.